Medical Physics Option : X-rays
For
details on the production of X-rays click here
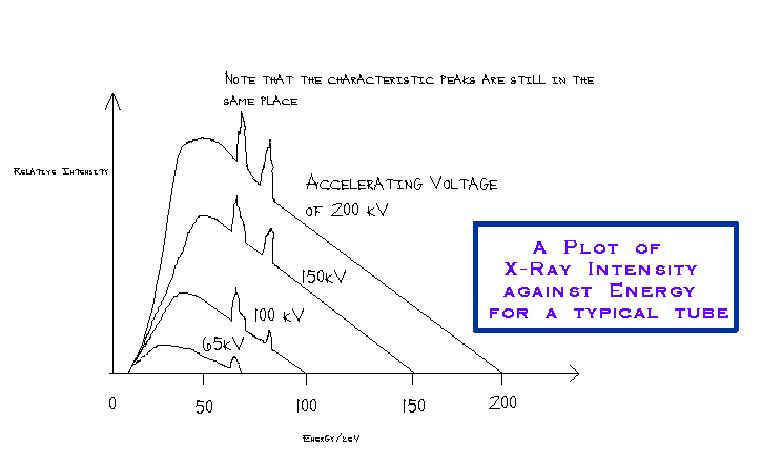
An ideal X-ray examination would produce a film that showed sufficient contrast between the features that the doctor wanted to examine while putting the patient at minimal risk from the ionizing effect of the radiation. An
X-ray tube does not produce a monochromatic beam, it produces a spectrum
of X-ray energies limited at the high energy end by the accelerating
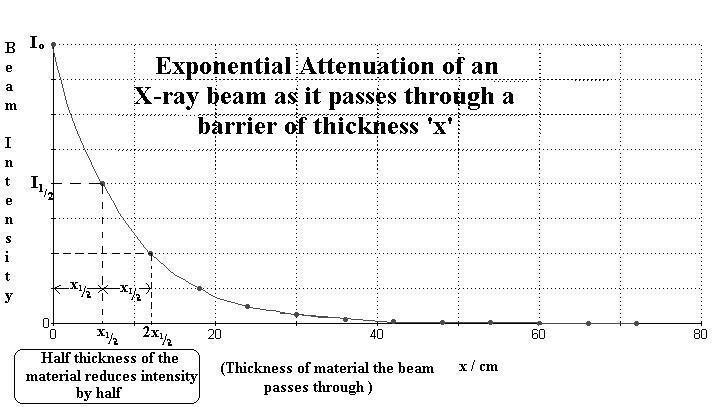
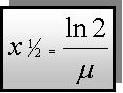
voltage applied. Attenuation (reduction of the beam strength) occurs as the X-rays pass through matter. This attenuation is exponential. Let then (in data book)Io = Intensity of the incident beam
I
= Ioe-m
x
Ensure
you can calculate half thicknesses as well as find them off graphs.
In a similar way you can find out the thickness needed to reduce penetration
to a tenth etc. ( put I = 0.1 Io into the equation). Values for the mass attenuation coefficient mm can be changed into m by using the equation mm = m / r The
lower energy rays are more likely to be attenuated by the body than
the high energy ones. Attenuation occurs as the radiation passes through
the body of the patient by two principal mechanisms: photoelectric
absorption and Compton scattering. Photoelectric absorption occurs when a photon of energy is absorbed by an orbital electron and this electron is then promoted to a higher energy level (more outer orbit) or leaves the influence of the nucleus completely (ionization). A.H.
Compton discovered that if he bombarded graphite with monochromatic X-rays,
the scattered X-rays had lower energies (longer wavelengths) than the
undeflected ones: the greater the deflection the bigger the energy loss.
The bombarding X-ray photon has a lot of energy - the force binding the
electron to the atom is insignificant compared to the force exerted by
the photon on impact. When the photon 'bounces off' the electron, the
electron recoils and thereby picks up some of the photon's energy. This
is called Compton Scattering. Photoelectric
absorption is the dominant mechanism for low energy X-ray photons (used
in soft tissue) whereas Compton Scattering becomes more significant for
higher energy photons (bone). Low
energy photon energies produce a better contrast between media of similar
density but overall absorption is greater. This means that a higher anode
current (resulting in a more intense beam) has to be used the lower the
accelerating potential employed across the tube. In a mammogram a typical range of X-ray energies would need to be in the region of 20-30 keV in order to get an image of sufficient contrast as the breast is composed primarily of fatty tissue. In a chest X-ray the densities of tissue to be investigated is much more diverse (bone/lung/heart) and 'harder' X-rays can be employed. These still give the contrast required in the image but absorption is reduced by using high energy rays and filtering out the lower energy ones (soft X-rays) produced by the tube. This can be done using an aluminium filter. Suitable energy for a chest X-ray would be 60-100 keV depending upon the exact nature of the detail required to make the diagnosis. Patient
doses
X-ray examinations of
Hence one CT scan is equivalent in dose to about 800 knee X-rays!! This
is why although many more low dose X-rays are carried out, they do not
contribute very much to the population dose. The much lower number of
major scans make a significant contribution to population dose because
they individually are equivalent to a vast number of low dose investigations.
The effective dose of each procedure varies because dose depends on: A real
time investigation such as Barium meal involves the patient being
bathed in X-rays as the doctor watches an image on a TV monitor. The dose
is minimized by pulse application and image freezing but necessarily involves
a much bigger dose than a simple 'snapshot' method as used in a chest X-ray.
The dose varies in its effect on tissue too as this is dependent upon the
quantity of cell division taking place and summed absorption of layers of
tissue (see variation in CT Scan doses for head and chest). LOJ
(October 2000) revised December 2002
|
Follow me...
|