|
Resolution of the eye or Visual acuity
Visual acuity describes the fineness of detail discernible by the eye.
Suppose two points of light are moved steadily apart until they are seen as separate (just resolved). Let the angle they subtend at the eye be  minutes. Then the visual acuity is 1/ minutes. Then the visual acuity is 1/ per minute. per minute.
Factors thst influence the eye's visual acuity:
 The optical system The optical system
- Some blurring of retinal images always occurs due to:
(i) aberrations which increase with increasing pupil size as the outer part of the cornea/lens is then used;
(ii) diffraction of light as it passes through the pupil. Diffraction increases as pupil size decreases. Therefore, the retinal image of a distant point source of light is a spot - bright at the centre and fading out towards blurred edges. The best compromise between aberrations and diffraction occurs with a pupil diameter of about 4 mm, and this then leads to a retinal spot diameter of about 10  m. m.
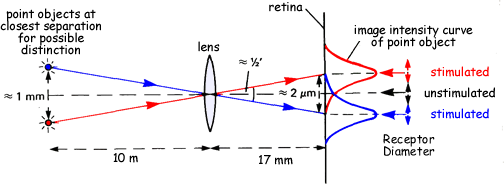
When two distant point sources are observed the resulting retinal images may overlap. Using Rayleigh's criterion, these images are just resolved if the maximum of one image intensity curve falls on the first minimum of the other image intensity curve.
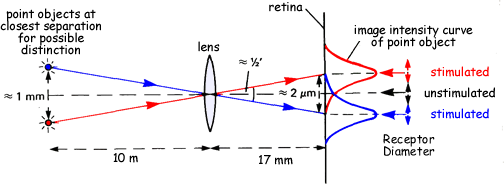
Under optimum conditions, this occurs for a distance between the centres of the retinal spots of about 2  m, and corresponds to an angular resolution of just less than half a minute. If two point sources are positioned about 10 m from the eye, about 1 mm apart they subtend approximately this angle at the eye and are just resolved by the optical system. m, and corresponds to an angular resolution of just less than half a minute. If two point sources are positioned about 10 m from the eye, about 1 mm apart they subtend approximately this angle at the eye and are just resolved by the optical system.
 The response system The response system
- If the separation between two adjacent retinal spots is to be perceived, there must be a receptor present in the intervening non-stimulated area. (See the diagram).
- There must also be adequate illumination to ensure stimulation of the relevant receptors and the mosaic of retinal receptors must have a sufficiently fine structure to record the resolved images of the optical system.
- So, a minimum perceivable separation corresponds to a spacing of at least two receptor diameters. At the fovea, the cone diameter averages about 1.5 μm and each cone has its own associated nerve fibre. Since there are only cones present here, a separation of about 3 μm can be perceived, corresponding to a visual angle of just over half a minute. At the periphery of the retina the separation is greater therefore less detail can be detected.
- At the fovea the resolving power of the optical system approximately matches that of the receptor system providing an angular limit of resolution of about half a minute, and therefore a visual acuity of about 2 per minute.
As the image moves away from the fovea, the visual acuity for photopic vision decreases rapidly.
This is due partly to the increased aberrations associated with oblique refraction, but mainly due to the increased sharing of nerve fibres by the receptors.
There are approximately 6 million cones and 125 million rods in the human retina, and these have to share about a million nerve fibres of the optic nerve. More sharing is done by the rods and also more sharing occurs at the retinal periphery. Hence, the allocation of nerve fibres goes from one per cone at the fovea to about one per 600 rods at the periphery. The photopic visual acuity, therefore, varies from about 2 per minute at the fovea to about 1 per minute just outside the fovea to about 0.05 per minute at the retinal border. Standard photopic visual acuity is taken to be about 1 per minute.
In contrast to this, for scotopic vision the fovea is inactive and the region just beyond it gives maximum visual acuity.
Peripheral vision is best in very weak light
This is due to the maximum convergence of rods onto nerve fibres. For example, when astronomers wish to detect very faint stars they 'look off' the fovea so that the image falls towards the retinal periphery. On average, scotopic visual acuity is about 0.1 per minute.
See a sample question - Q7 on this page of past paper questions.
|






 The optical system
The optical system